- Tricare Standard Copays And Deductibles
- Tricare Standard Copay 2019
- Tricare Standard Copays And Deductibles
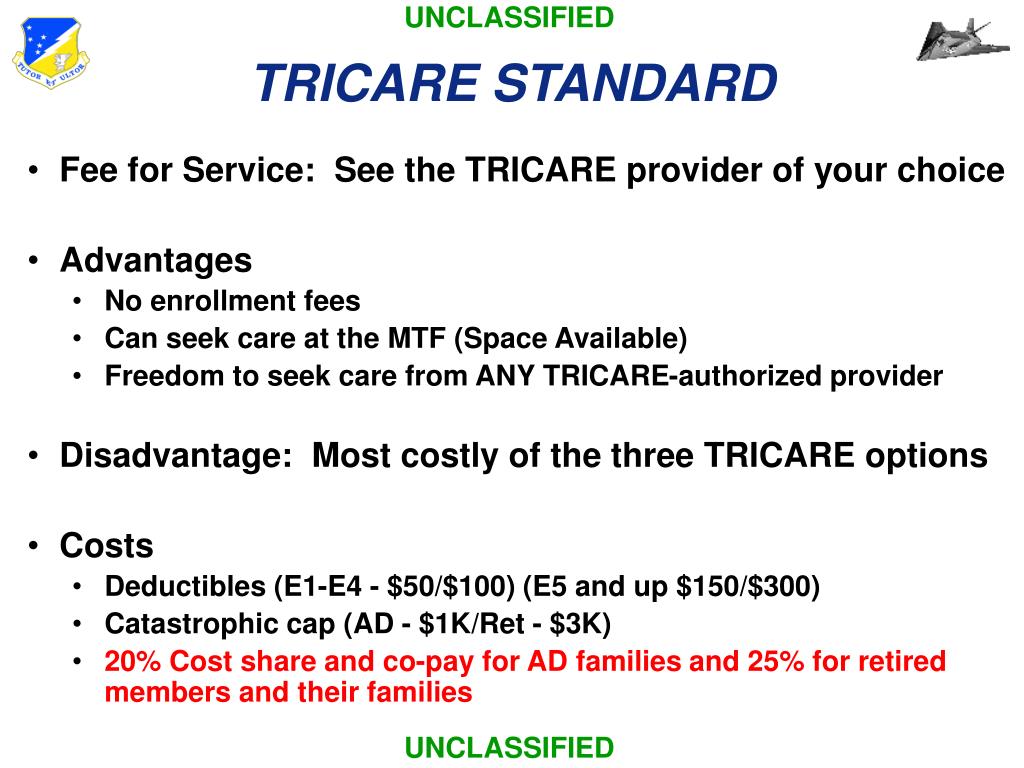
Starting on Jan. 1, 2021, TRICARE Select Group A retired beneficiaries must pay monthly enrollment fees in order to maintain their TRICARE health coverage. This is a change, and the first time this beneficiary group will pay enrollment fees. TRICARE Prime TRICARE Select; Active Duty Family Members: Retiree Family Members: Active Duty Family Members: Retiree Family Members: $0: $0: 2020: E4 and Below: $52/individual E5 and Above: $156/individual. 2021: E4 and Below: $52/individual E5 and Above: $158/individual. 2020: Network Providers: $156/individual Non-Network Providers: $313/individual. 2021: Network Providers.
Covered Services
Learn more about what we cover -including health, dental, and pharmacy.

On Jan. 1, some copayments for your prescription drugs will increase. If you get your prescriptions through the TRICARE Pharmacy Home Delivery or at a retail network pharmacy, you’ll pay anywhere from $2 to $7 more starting Jan. 1. Congress made this change in the National Defense Authorization Act for Fiscal YearOctober 1 - September 30 2018.
There’s still no cost to fill your prescriptions at military pharmacies. Microsoft teams versus slack. And these cost changes don’t apply to active duty service members (ADSMs). If you’re an ADSM, you still pay nothing for your covered drugs at military and network pharmacies.
“Military pharmacies remain to be your lowest cost option,” said U.S. Air Force Lt. Col. Melissa Pammer with the Pharmacy Operations Division at the Defense Health Agency. “Your next lowest cost is if you use the TRICARE Pharmacy Home Delivery.”
TRICARE Prescription Drug Categories
Your prescription copayments vary based on pharmacy type. Also, they vary based on the drug category. TRICARE groups prescription drugs into one of four categories. This grouping is based on the medical and cost effectiveness of a drug compared to other drugs of the same type.
As outlined in the TRICARE Pharmacy Program Handbook, the drug categories include:
- Generic formulary drugs: These drugs are widely available. You have the lowest out-of-pocket costs for these drugs.
- Brand-name formulary drugs: These drugs are generally available to you. Plus, they offer you the second lowest copaymentA fixed dollar amount you may pay for a covered health care service or drug..
- Non-formulary drugsA drug in a therapeutic class that isn’t as clinically or cost-effective as other drugs in the same class. You pay a higher cost share for these drugs.: These drugs may have limited availability. You have higher copayments for these drugs. Also, there’s generally an alternative formulary drug that you can get. It’s often more cost effective, and equally or more clinically effective.
- Non-covered drugs: TRICARE doesn’t cover these drugs. If you choose to purchase a non-covered drug, you’ll pay 100% of the drug’s cost. These drugs are either not clinically effective, or as cost effective as other drugs offered. They may also pose a significant safety risk that may outweigh any potential clinical benefit.
To learn more, you can download the TRICARE Pharmacy Program Handbook from the Publications page.
Pharmacy Copayment Increases
TRICARE Pharmacy Home Delivery
If you use home delivery, your copayments for up to a 90-day supply of generic formulary drugs will increase from $7 to $10. For brand-name formulary drugs, your copayments will increase from $24 to $29. Your copayments for non-formulary drugs when you don’t have a medical necessity will increase from $53 to $60.
TRICARE retail network pharmacies
At a retail network pharmacy, your copayments for up to a 30-day supply of generic formulary drugs will increase from $11 to $13. For brand-name formulary drugs, the increase is from $28 to $33. Non-formulary drugs will increase from $53 to $60.
Non-network pharmacies
At a non-network pharmacy, you must pay the full price of the drug. After meeting your annual deductible, you may submit a claim for partial reimbursement. Non-network pharmacy costs remain the same if you use TRICARE Prime. With TRICARE Prime, you’ll pay a 50% cost-shareA percentage of the total cost of a covered health care service that you pay. after meeting your point-of-service deductible for covered drugs.
For all other health plans, non-network pharmacy costs are as follows:
- Generic formulary drugs and brand-name formulary drugs will cost $33 (up from $28) or 20% of the total cost, whichever is more, after you meet your annual deductible.
- Non-formulary drugs will cost $60 (up from $53) or 20% of the total cost, whichever is more, after you meet your annual deductible.
Tricare Standard Copays And Deductibles
Copayments for survivors of ADSMs are the same as the 2017 rates. The copayments remain the same for medically retired service members and their family members, too.

For the latest TRICARE pharmacy costs, you should visit TRICARE Costs. To learn more about your pharmacy benefit, visit Pharmacy on the TRICARE website.
Last Updated 2/17/2021
Costs
Find your TRICARE costs, including copayments,enrollment fees, and payment options.
- Most costs are for calendar year 2021 unless noted separately.
- For US Family Health Plan and TRICARE Prime Remote costs, choose 'TRICARE Prime' from the pull-down menu
- Visit the Cost Terms page for definitions to help you better understand TRICARE costs.
- If you're an unremarried former spouse, for the Continued Health Care Benefit Program (CHCBP), chose 'Retired' regardless of your sponsor's status
- Looking for dental costs? Visit the TRICARE Dental Costs section.
Tricare Standard Copay 2019
Tricare Standard Copays And Deductibles
Copayments will be waived retroactively to March 18 for certain testing and office visits related to the testing. The test must be one approved, cleared, or authorized by the Food and Drug Administration to detect SARS-CoV-2 or diagnose COVID-19. If you paid any copayments for testing related to COVID-19 and the resulting office visits with a network or non- network provider, you may file a claim for reimbursement. For more information related to the coronavirus, visit the FAQ page.
