Covered Services
Copayments and Cost-Shares TRICARE is waiving copayments and cost-shares for covered audio-only or video telemedicine rendered by network providers on or after May 12, 2020. This waiver applies to covered in-network telehealth services, not just services related to COVID-19. TRICARE covers the use of secure video conferencing to provide medically necessary services. You connect securely with a provider using a computer or smartphone. This includes for certain: Office visits Preventive health screenings Telemental health services (individual psychotherapy, psychiatric diagnostic interviews and exams, and medication management) Services for End Stage Renal Disease. Telehealth is allowed using a HIPAA compliant real-time audio/video conferencing service or audio only, using Place of Service 02 and modifier '95'. Providers must be in network. Telehealth services must be a covered benefit under the member’s benefit plan. Copays/Coinsurance Waiver: Yes, until.
Learn more about what we cover -including health, dental, and pharmacy.
TRICARE covers the use of secure video conferencing to provide medically necessaryTo be medically necessary means it is appropriate, reasonable, and adequate for your condition. services. You connect securely with a provider using a computer or smartphone. Jds uniphase port devices driver download for windows 10. This includes for certain:
- Office visits
- Preventive health screenings
- Telemental health services (individual psychotherapy, psychiatric diagnostic interviews and exams, and medication management)
- Services for End Stage Renal Disease
Using Telemedicine Services
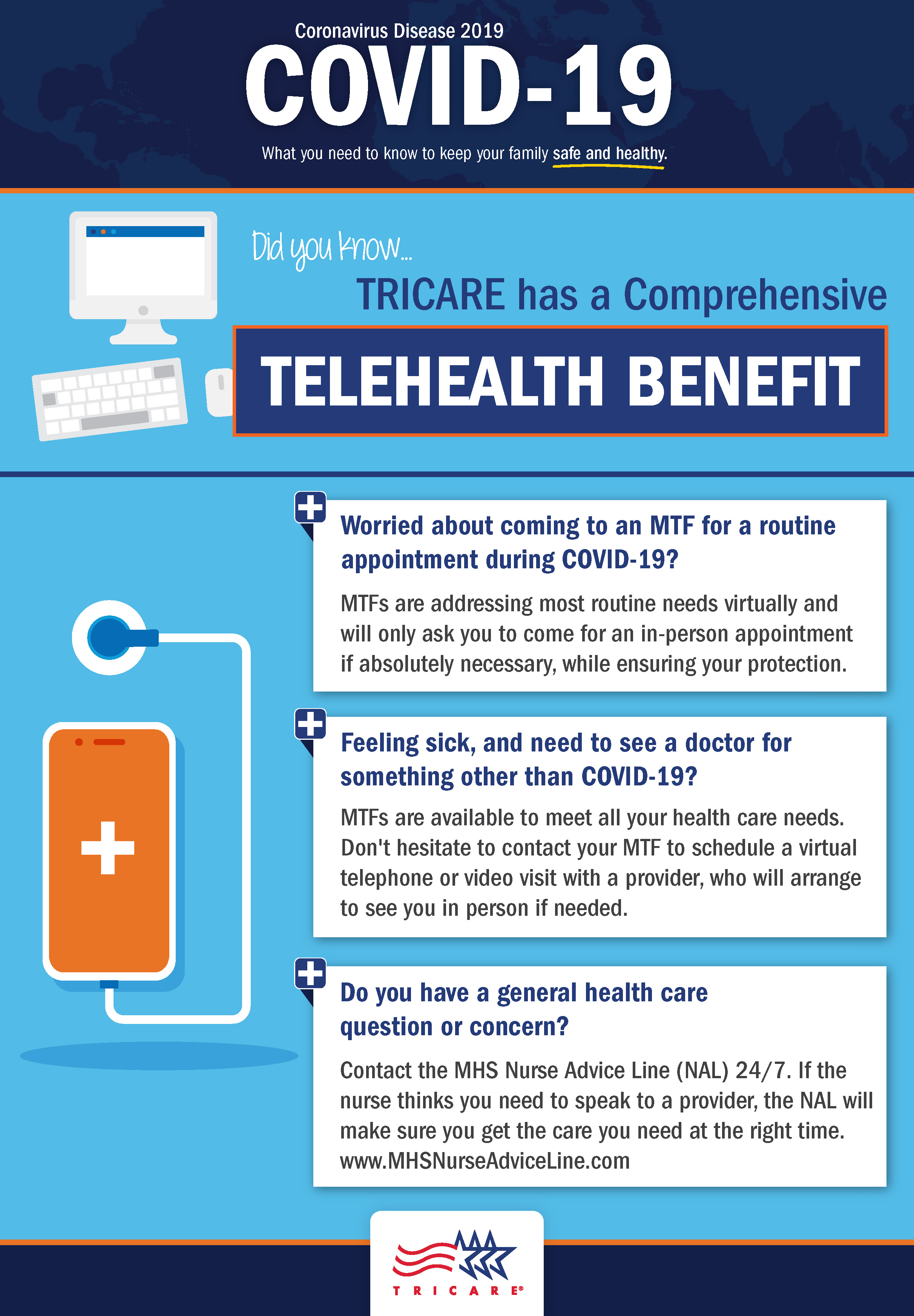
Depending on your TRICARE plan, you may first need an authorization or referral. Contact your regional contractor. Active duty service members need a referral for telemental health care.
TRICARE recently revised its policy on telemedicine services. These changes are temporary during the national health emergency due to the pandemic. TRICARE will now:
- Cover audio-only telemedicine visits.
- Waive cost-shares and copayments for all covered telemedicine services. These services must be from a military provider or TRICARE network provider.
- Allow more providers to offer telemedicine services. Some providers may not offer this service, so be sure to ask.
- If you're overseas, the country where you live must allow telemedicine. The provider also must be licensed to practice where you live. Contact your TOP Regional Call Center for more information, including provider eligibility.
If you use TRICARE For Life, Medicare should cover telemedicine visits when the service and provider are payable by Medicare. This temporarily includes audio-only telemedicine visits. If they aren't payable by Medicare, TRICARE For Life will process as first payer. Deductibles and cost-shares will then apply. Learn more about Medicare coverage.
As of Mar. Usb network gate mac waiting for daemon to launch. 31, 2020, TRICARE covers telehealth care for applied behavior analysis (ABA) parent or caregiver guidance services under the Autism Care Demonstration. This is an ongoing temporary change during the national health emergency due to the pandemic
This list of covered services is not all inclusive. TRICARE covers services that are medically necessary and considered proven. There are special rules or limits on certain services, and some services are excluded.

Last Updated 8/24/2020
Find a Doctor
Prescriptions
Vision
Mental Health Therapeutic Services
See our Telemedicine Services page for benefit information and approval requirements.

Synchronous Telemedicine Services
Tricare Telemedicine Copay
Synchronous telemedicine services involve an interactive, electronic information exchange in at least two directions in the same time period.
Providers must bill using CPT® or HCPCS codes with a GT or 95 modifier for distant site and Q3014 for an applicable originating site to distinguish telemedicine services. Payment for Q3014 will not be made when a patient's home is the originating site. The distant site and originating site cannot be billed by the same provider.
For professional claims, use the place of service code (POS) that represents the location from which he/she rendered the telemedicine visit. For example, POS 11 if services are rendered from the provider's office.
Tricare West Telehealth
- Exception: At this time, applied behavior analysis (ABA) claims continue to require the appropriate telemedicine modifier and POS 02 for all telemedicine claims.
- See FAQs below for information on resubmitting non-facility claims previously submitted with POS 02.
By billing the GT or 95 modifier with a covered telemedicine procedure code, the distant site provider certifies the beneficiary was present at an eligible originating site when the telemedicine service was furnished.
Asynchronous Telemedicine Services
Asynchronous telemedicine services involve storing, forwarding and transmitting medical information on telemedicine encounters in one direction at a time.

Providers must bill using CPT or HCPCS codes with a GQ modifier. For professional claims, use the place of service code (POS) that represents the location from which he/she rendered the telemedicine visit. For example, POS 11 if services are rendered from the provider's office. However, at this time, ABA claims continue to require the appropriate telemedicine modifier and POS 02 for all telemedicine claims.
Note: When submitting claims for telemedicine services, the originating site provider may indicate 'Signature not required – distance telemedicine site' in the required Patient Signature field.
